A new study has reignited an intriguing scientific discussion. It suggests that the herpes simplex virus type 1 (HSV-1), commonly known for causing cold sores, may be connected to the development of Alzheimer’s disease.
This concept isn’t entirely novel. Previous research has hinted at an association between HSV-1 and Alzheimer’s, the most prevalent form of dementia. This latest research provides additional data, prompting a closer look at the strength and implications of this potential link.
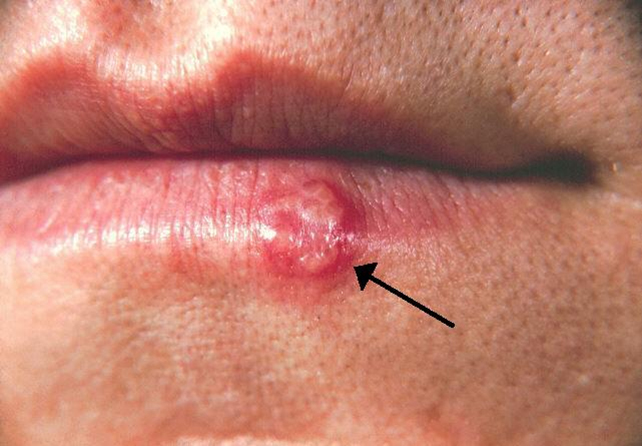
Understanding HSV-1: A Common Neurological Virus
Before delving into the new findings, it’s important to grasp what HSV-1 is and how it operates within the human body.
A Highly Prevalent Neurotropic Virus
HSV-1 is classified as a neurotropic virus. This means it possesses the unique ability to infect nerve cells. These specialized cells are crucial for transmitting and receiving messages throughout the brain and nervous system. The virus is exceptionally common globally. The World Health Organization estimates that nearly two-thirds of the global population under 50 carries HSV-1. Often, individuals are unaware they are carriers.
Initial Infection and Dormancy
An initial HSV-1 infection can present with a range of symptoms. These may include mild to severe manifestations such as fever, headache, and muscle aches. It can also cause characteristic blisters and ulcers around the mouth or lips. After this initial symptomatic phase, HSV-1 typically enters a state of dormancy. It then resides silently within the body’s nervous system.
The virus can, however, reactivate periodically. This reactivation is often triggered by factors like stress or illness. During reactivation, HSV-1 can cause recurrent symptoms such as cold sores. Importantly, in many individuals, the virus remains asymptomatic even during reactivation.
The New Research: A Look at the Evidence
Published in BMJ Open this week, the latest study delves into a large dataset to explore the HSV-1 and Alzheimer’s connection.
Analyzing Extensive Health Insurance Data
Researchers conducted a detailed analysis of data drawn from hundreds of thousands of people. This extensive dataset originated from a large United States health insurance system. The study employed a matched “case-control” analysis. It involved over 340,000 adults aged 50 and older. All these individuals had received an Alzheimer’s disease diagnosis between 2006 and 2021.
To ensure statistical rigor and minimize bias, each Alzheimer’s patient (a “case”) was carefully matched with a control individual. These controls did not have an Alzheimer’s diagnosis. Matching was based on crucial factors such as age, sex, and geographic region.
Key Findings: Increased Risk and Antiviral Impact
The research team then meticulously examined the medical records of these individuals. They investigated how many had a prior diagnosis of HSV-1. Crucially, they also looked at whether these individuals had been prescribed antiviral treatment for the infection.
The findings revealed a notable difference. Among people diagnosed with Alzheimer’s disease, 0.44% had a previous HSV-1 diagnosis. This contrasted with 0.24% of the control group. This difference translates to an 80% increased relative risk of Alzheimer’s disease in those previously diagnosed with HSV-1.
However, it’s vital to note that the absolute numbers of diagnosed HSV-1 cases within both groups were relatively small. This indicates that while the relative risk is higher, the direct diagnosis of HSV-1 in these datasets is not overwhelmingly common.
Furthermore, the study uncovered another significant detail. People who had received antiviral treatment for HSV-1 showed a roughly 17% lower risk of developing Alzheimer’s disease. This was compared to those who remained untreated for the viral infection. This finding suggests a potential protective effect of antiviral medications.
The “Herpes Hypothesis”: Past Research and Important Caveats
The idea of a viral role in Alzheimer’s is not new, but crucial distinctions must be made between association and causation.
Prior Research and Amyloid-Beta Accumulation
This isn’t the first time researchers have speculated about a viral contribution to Alzheimer’s disease. Earlier studies have indeed detected HSV-1 DNA in postmortem brain tissues from individuals who had Alzheimer’s disease. This provided early biological clues. Laboratory research has also demonstrated that HSV-1 can trigger amyloid-beta plaque accumulation in nerve cells and even in mouse brains.
Amyloid-beta plaques are one of the hallmark pathological features of Alzheimer’s disease. This laboratory evidence has led to speculation that repeated reactivation of the virus might contribute to chronic brain inflammation or direct neuronal damage, potentially accelerating the disease process.
Association, Not Causation
Despite these compelling links, it is extremely important to emphasize a critical point: both previous research and the current study show associations, not definitive proof that HSV-1 directly causes Alzheimer’s disease. These observed links do not confirm that the virus initiates or actively drives the progression of the disease. Alzheimer’s is a complex condition, and a virus might be a contributing factor rather than the sole instigator.
Limitations of Insurance Claim Data
The study’s reliance on insurance claim data introduces several important caveats. Such data may not always perfectly reflect accurate or timely clinical diagnoses. Furthermore, HSV-1 is frequently underdiagnosed in the general population, especially when symptoms are mild or entirely absent.
These factors could explain why both the Alzheimer’s group and the control group in the study showed such low rates of recorded HSV-1. Population rates for this virus are estimated to be significantly higher. This discrepancy means that many HSV-1 carriers within the study might have gone unrecorded. This makes the interpretation of the observed link more challenging and less clear-cut.
Additionally, the dataset does not capture crucial details like the frequency, severity, or duration of recurring HSV-1 symptoms. These factors might directly influence the risk of Alzheimer’s disease.
Other Contributing Factors
Another complicating factor is the potential for other differences between people with HSV-1 and those without it. Variations in health-care access, the strength of an individual’s immune system, specific lifestyle choices, genetic predispositions, or even educational attainment could all independently influence Alzheimer’s disease risk. These confounding variables make it difficult to isolate the precise impact of HSV-1 alone.
Implications for Individuals: Should Cold Sores Be a Concern?
Given these findings, it’s natural to wonder if having cold sores should be a cause for concern regarding Alzheimer’s risk.
No Need for Alarm for Most Individuals
The short answer is no, not based on current evidence. The vast majority of people with HSV-1 will never develop Alzheimer’s disease. The overwhelming majority of individuals live with the virus throughout their lives without experiencing any serious neurological issues or cognitive decline.
While the “herpes hypothesis” of Alzheimer’s disease represents an interesting and promising area for further scientific research, it is far from being settled science. This new study certainly adds weight to the ongoing scientific conversation. However, it does not offer a definitive answer or a direct causal link that should alarm the general public.
A Complex Disease with Multiple Risk Factors
It is crucial to remember that Alzheimer’s disease is a profoundly complex condition. Its development is influenced by a multitude of interconnected risk factors. These include significant factors such as age, genetic predisposition, overall heart health, educational background, various lifestyle choices, and environmental exposures.
Infections like HSV-1 may indeed represent one piece of this intricate, larger puzzle. However, they are highly unlikely to be the sole cause or the primary driver of the disease.
Focusing on Established Brain Health Strategies
With this understanding, the most effective course of action for individuals is to concentrate on what is already scientifically known to promote long-term brain health as they age. Proven strategies include:
- Regular physical activity: Exercise significantly benefits cognitive function and overall brain health.
- Good quality sleep: Adequate and restorative sleep is crucial for memory consolidation and brain repair.
- Social engagement: Maintaining strong social connections and intellectual stimulation can help build cognitive reserve.
- A balanced diet: A nutritious diet, often rich in fruits, vegetables, and healthy fats, supports brain function.
- Managing stress: Chronic stress can negatively impact brain health, making stress reduction techniques important.
By prioritizing these established health practices, individuals can proactively support their cognitive well-being.